Adherence at Scale Starts with the Point of Care
by Ashli Sherman
The Point of Care Practice has been incredibly active so far this year. One of our newest opportunities for engagement has been in the health systems space, reaching both clinicians and patients.
In 2020, Ogilvy Health began a collaboration with Medicom Health on a novel approach to helping US-based healthcare providers improve medication adherence at scale.
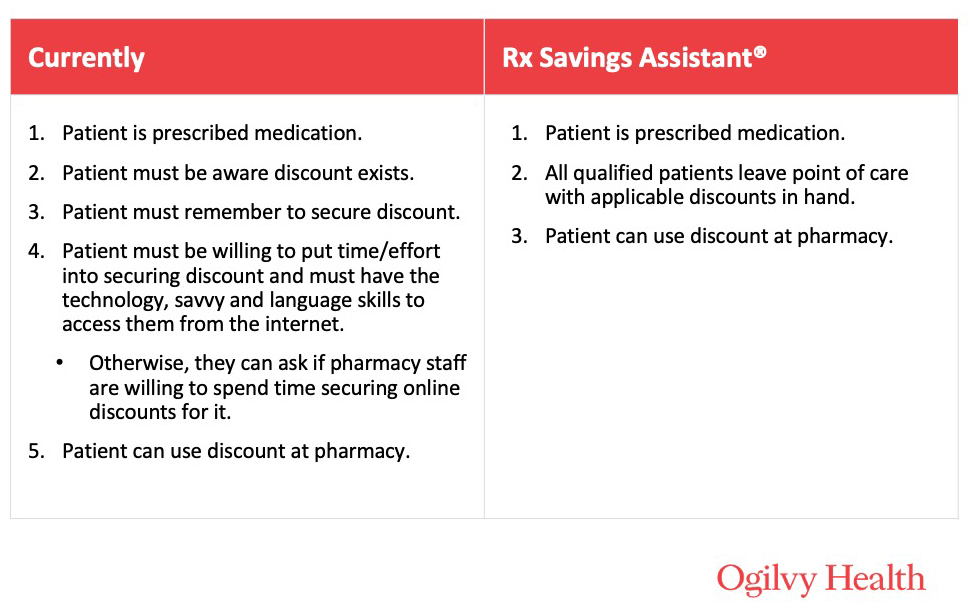
Medicom Health’s new technology, Rx Savings Assistant®, is a plug-in for Electronic Health Record (EHR) systems, such as Epic and Cerner, that can radically increase the availability and use of branded prescription discounts across an enterprise, lowering patient medication costs. Patients may be segmented by commercial or government insurance or cash.
A recent study shows 22% of nonadherent patients say “trying to save money” is a major reason for not filling a prescription.
A recent study shows 22% of nonadherent patients say “trying to save money” is a major reason for not filling a prescription. That number is likely significantly higher now, given the financial devastation of COVID-19. Research also shows that manufacturer discounts can help improve adherence, but are woefully underutilized, considering the addressable market. Automation at the point of care has become a real game changer.
Automation at the point of care has become a real game changer.
The technology invisibly “listens” for every new prescription in both acute and ambulatory practice settings, finds appropriate discounts in multiple databases, and automatically embeds the discount into the printed paper discharge report, electronic patient record and patient portal for every qualified patient. No apps, no impact on prescribing, no change to workflows. Discounts can include patient support programs, savings offers, enrollment forms, and even free prescription trial offers. Ogilvy’s extensive relationships with pharma manufacturers ensures the solution has access to plenty of quality discounts.
Although the process requires no effort on the clinician beyond writing the script, clinicians are informed the offers are available for their patients at the onset of the program, with reminders available to them throughout the program. The printed offers are shared with the patient at discharge and are also available online in their health portal—so telehealth visits in no way prevent the patient from receiving the offer.
Today, 9 leading health systems already use this solution, and it’s expected to be live in 20 health systems before the end of the year. Many of the 900+ hospitals that work with Medicom Health are exploring the program now.
This new, strategic approach is already showing remarkable results. We’ll be sure to report back as adherence program metrics come in.
Interested in learning more about how digital solutions are improving point of care experiences? Check out our expert’s POV on how real-time benefit checks are facilitating critical financial conversations at the point of care.